Case: A 52-year-old female presents to your ED after sustaining a car accident loosing control of her vehicle on the ice. She was belted and experienced a head-on collision with incoming traffic. She presented to the ER with excruciating body pains in a c-spine collar. You notice her right leg is internally rotated and shortened. After resuscitating the patient, what comes next?
Take Home points
- Usually hip dislocations occur when a large axial force is applied but patients with an artificial hip or hip arthroplasty may present with a relatively benign mechanism of injury.
- 90% are posterior dislocations.
- Treatment is usually non-operative with emergent closed reduction within 6 hours to prevent avascular necrosis of the femoral head and sciatic nerve injury.
- If there is an associated fracture of the femoral neck, reduction should not be attempted by the ER physician and Orthopedics should be consulted.
- For Prosthetic hip dislocations Orthopedics should be consulted and involved in the Emergency Department.
- Several reduction techniques exist and a few are described in this article.
- Don’t forget to look for associated injuries as the forces required to dislocate a hip usually are of great magnitude and the patient often presents with concomitant injuries.
1 . Mechanism and Presentation
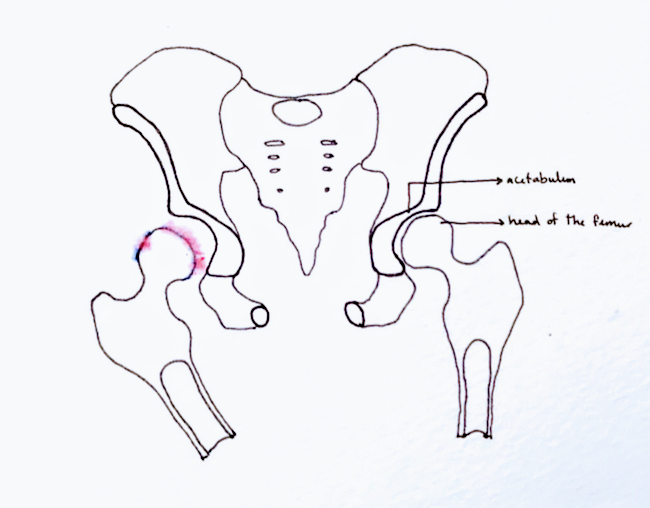
The hip is a ball-and-socket joint and can be disrupted when a large axial force is applied, dislocating the joint out of it’s socket. This is particularly true when the hip is flexed and ADDucted (ie, motor vehicle accidents, pedestrians struck by automobiles). Hip dislocations can also occur in high-energy impact athletic events. Patients with an artificial hip or hip arthroplasty on the other hand can present with a relatively benign mechanism of injury. Due to the anatomy, posterior hip dislocation is far more common than anterior dislocation and account for 90% of all hip dislocations.
Patients who sustain a hip dislocation present with severe hip pain and an inability to weight bear which may or may not be accompanied by motor or sensory deficits. On exam, the patient most commonly presents with the hip and leg in slight flexion, ADDuction and internal rotation which suggest a posterior dislocation. The patient may present with hip and leg flexion, ABDuction and external rotation, which suggest an anterior dislocation. Pulses and peripheral perfusion should be assessed as well as neurological function. The sciatic nerve is particularly at risk and can be tested by assessing foot sensation and motor function with ankle plantar and dorsiflexion. A sensory deficit over the antero-medial thigh should raise suspicion of a femoral nerve injury.
2. Imaging
Plain X-rays of the hip in AP and cross-table lateral view is used for diagnosis. Clues for a dislocation are :
- Loss of congruence of the femoral head with the acetabulum.
- A disruption of Shenton’s line (seen below).
- In posterior dislocation the lesser trochanter is not visible whereas in anterior dislocation the lesser trochanter is more visible.
- In posterior dislocation, the femoral head is usually smaller when compared to the adjacent hip. It appears larger then the adjacent hip in anterior dislocation.
- The most common associated fracture is a fracture of the posterior wall of the acetabulum (in a posterior luxation) and a fracture of the anterior wall of the acetabulum (in an anterior luxation).
3. Treatment
Treatment is usually non-operative with emergent closed reduction within 6 hours to prevent avascular necrosis of the femoral head and sciatic nerve injury.
For Prosthetic hip dislocations, Orthopedics should be consulted in the Emergency Department. Depending on the prosthetic materials and post-operative timing, some may need to be revised with operative management.
Operative management is needed in cases of irreducible dislocations, radiological evidence of fractures of the femoral head or intra-articular fragments, as well as in delayed presentations.
4. Reduction Techniques
To ensure successful reduction it is recommended the patient be properly sedated throughout.
Captain Morgan Technique
The physician foot is placed at 90 degrees, perpendicular to the patient’s affected side, under the patient’s hip. Ideally this is done on a firm surface (i.e. backboard of the stretcher). This position mimics Captain Morgan standing with one leg up against a barrel, giving the technique it’s colorful name. The patient’s leg is then bent 90 degrees at the hip and knee in flexion. The patient’s knee is placed on the physician’s knee, which acts as a lever for the physician to apply traction. The physician then places one hand under the patient’s knee, lifting up the femur, and the other over the patient’s ankle, pushing it downwards. Another set of hands can stabilize the pelvis during this maneuver. This traction and leverage maneuver allows for the posterior hip to be reduced back into its socket anteriorly.
The Whisler Technique
Similar to the Captain Morgen but the forearm of the physician is used rather then the knee. The forearm is placed under the affected leg in the popliteal fossa and the hand grasps the knee of the unaffected leg. Positioning and traction maneuvers are the same as described above.
The Allis Maneuver
The patient is supine while the physician climbs on the stretcher, placing the patient’s affected leg between the physician’s knees with the patient’s hip and knee flexed at 90degrees. The physician then applies a traction force under the patient’s knee upwards using both hands while an assistant is stabilizing the pelvis. The patient’s hip should slide into the socket with the traction force alone.
Anterior Hip Dislocation
The physician applies a lateral traction on the affected side with an assistant stabilizing the pelvis. Once the femur head is over the acetabular opening, the hip is reduced by internally rotating the femur.
There are multiple other approaches to closed reduction, For more details, please see the article by Waddell et al. in the references.
5. Post-Reduction Management
After any reduction, the hip should be tested for proper range of motion. For native hips an xray and a CT-scan should be obtained to rule out any femoral head fractures or intra-articular loose bodies. For prosthetic hips an xray is often sufficient. The patient is then placed in a knee immobilizer to prevent flexion and re-dislocation and should be seen by Orthopedics in house.
Complications associated with hip dislocations are post-traumatic arthritis in 20% of dislocations, femoral head osteonecrosis in 5-40% of cases and sciatic nerve injuries in 8-20% of patients associated with longer time to reduction. Recurrent dislocations occur in less than 2% of cases.
Finally don’t forget to look for associated injuries as the forces required to dislocate a hip usually are of great magnitude and the patient often presents with concomitant injuries. Look for knee and patellar fractures and ligamentous injuries (a posterior cruciate ligament injury is also often associated with dashboard injuries).
References:
Hip Dislocation Treatment & Management. Medscape. 2018
https://emedicine.medscape.com/article/86930-overview
Hip Dislocation. Ortho Bullets. 2018
https://www.orthobullets.com/trauma/1035/hip-dislocation
THA Dislocation. Ortho Bullets. 2018
https://www.orthobullets.com/recon/5012/tha-dislocation
Trick of the Trade: Captain Morgan technique for hip dislocation. Academic Life in Emergency Medicine. 2011.
Waddell BS, Mohamed S, Glomset JT, Meyer MS. A Detailed Review of Hip Reduction Maneuvers: A Focus on Physician Safety and Introduction of the Waddell Technique. Orthop Rev (Pavia). 2016;8(1):6253. Published 2016 Mar 21. doi:10.4081/or.2016.6253
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4821229/
Written by: Madelaine Yona during her year as a CCFP-EM resident, Mcgill University
Reviewed by: Chanel Fortier-Tougas, Alexis Rousseau-Saine