A 46 year old male comes into the ED with acute knee pain and swelling after slipping on ice and falling from his own height.
This article will review the diagnostic approach and treatment of patellar and quadriceps tendon rupture.
Take home points:
– Patellar and quadriceps tendon rupture are clinical diagnosis
– They are commonly missed in the ER if we do not look for them
– Radiographs are often normal
– Inability to straight leg raise is key to the diagnosis
– They require urgent orthopedic consultation for operative repair
Mechanism and symptoms
These injuries most often occurs when there is a combination of knee flexion and quadriceps contraction. It may also occur from a fall on a flexed knee. In non-athletes it may occur when a person falls backward with their foot caught on the ground. The patient may experience a pop or tearing sensation. Usually, they present with diffuse swelling, difficulty weight bearing and severe pain.
Patients with patellar degeneration or tendinopathy, prior tendon repair, steroid injection or post total knee arthroplasty are all at higher risk for tendon rupture. A few medications are associated with tendon ruptures (ex: quinolones) and some systemic illnesses increase the risk of developing this injury (chronic renal failure, diabetes, rheumatoid arthritis, lupus, calcium pyrophosphate deposition disease). Quadriceps tendon rupture is more frequent in patients older than 40 years old while patellar tendon rupture occurs more commonly in individuals that are less than 40 years old. Finally, quadriceps tendon rupture is more common than patellar tendon rupture.
Physical exam and diagnosis
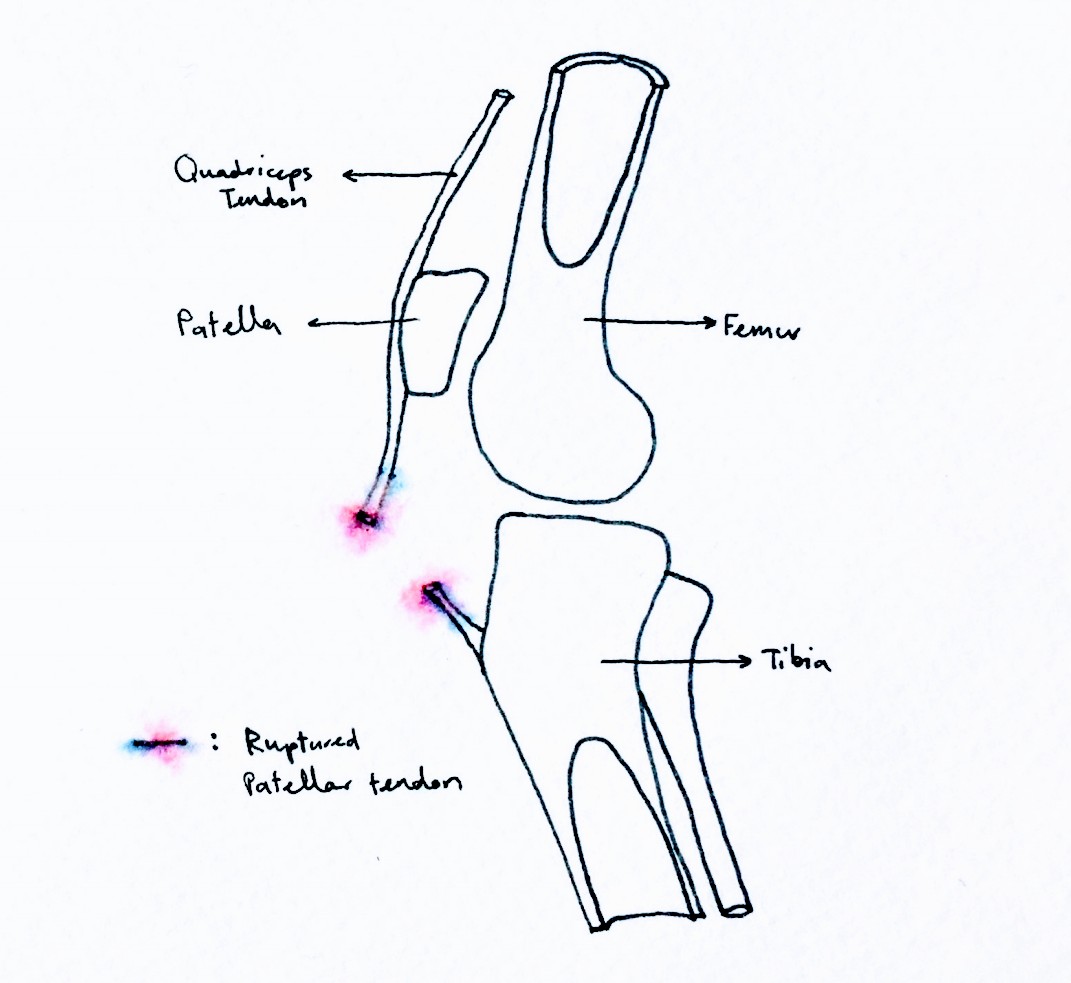
On physical exam the patient presents will present with diffuse swelling and localized pain usually above or below the patella. Feel for a palpable sulcus proximal to the patella (quadriceps tendon rupture) or distal to the patella (patellar tendon rupture). Look for a hypermobile or high riding patella.
The key feature to diagnoses quadriceps and patellar tendon rupture is the inability to perform a straight leg raise. Of note, the straight leg raise test is more sensitive in sitting position with knee flexed 90 degrees. This isolates the quadriceps function and avoids possible false positive maneuvers in the supine position.
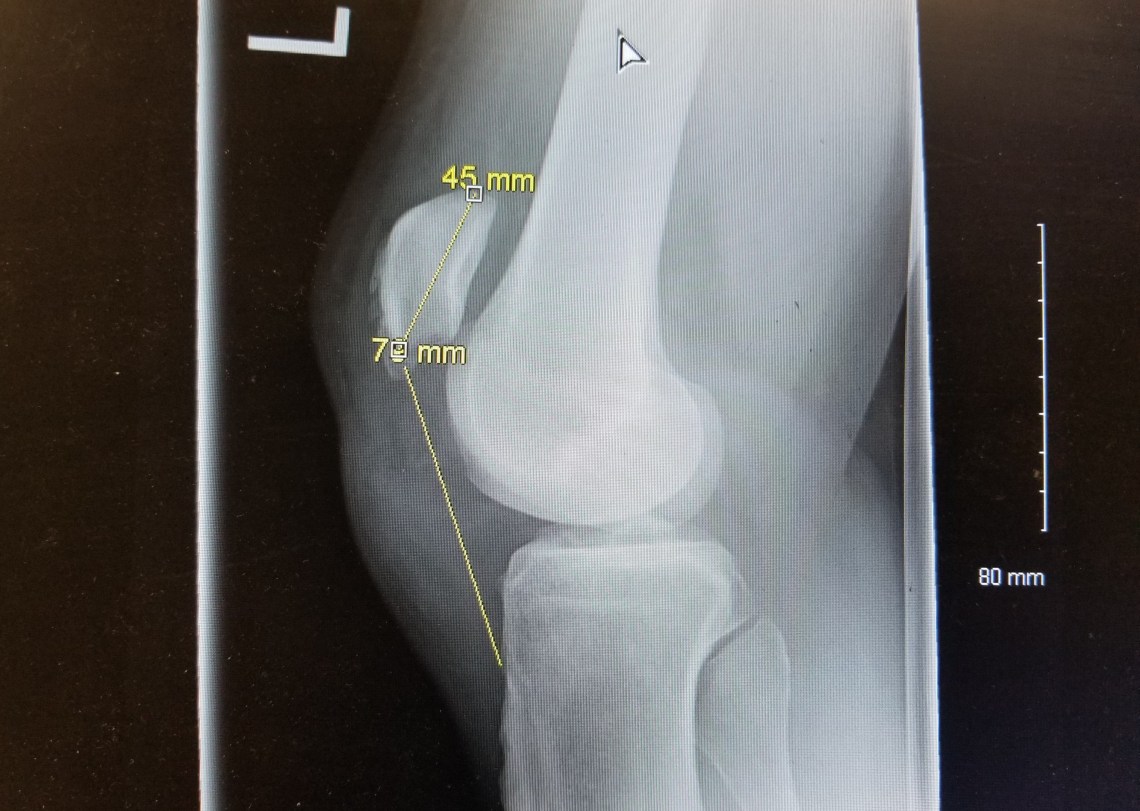
The radiographs are usually normal. In quadriceps rupture, an avulsion fracture of the superior pole of the patella may be seen whereas in patellar tendon rupture you may see a high-riding patella (Patella alta) on the lateral film. This can be appreciated using the Insall-Salvati ratio, where the patellar tendon length (distance from the lower pole of the patella to the tibial tuberosity) to patellar length (greatest pole-to-pole length) ratio is considered normal between 0.8 and 1.2. A ratio >1.2 is considered a patella alta, suggestive of patellar tendon rupture and a ratio <0.8 is considered a low riding patella, or patella baja, suggestive of quadriceps tendon rupture. This is best measured on lateral films with knee flexed 30 degrees.
This is a clinical diagnosis, but MRI or ultrasound can help differentiating a partial from a complete tear and helps in diagnosing associated soft tissue injuries.
Treatment
Complete tears or partial tears with a non competent extensor mecanism warrants an orthopaedic consultation in the Emergency Department for operative repair. The affected knee should be immobilized in full extension with a zimmer splint and the patient should be advised to remain non-weight bearing. Early surgical repair is necessary to ensure good functional outcomes.
Incomplete tears with intact extensor mechanisms can be treated with immobilization (Zimmer splint) in full extension and close follow-up.
Return on the case
The patient had an inability to straight leg raise, a palpable infrapatellar sulcus and a high riding patella on his radiograph. He was diagnosed with complete patellar tendon tear and orthopaedics were consulted in house for operative repair.
Written by: Samantha Thonnard Karn, CCFP-EM resident, McGill University
Edited by: Chanel Fortier-Tougas, Alexis Rousseau-Seine
References:
1. Bartelena, T. et al. Patellar Tendon Rupture: Radiologic and Ultrasonographic Findings. West J Emerg Med. Feb 2010.
2. Thurston M. et al. Patellar Tendon Rupture. Radiopaedia. Retrieved April 2 2019. https://radiopaedia.org/articles/patellar-tendon-rupture
3. Timothy J. Von Fange. Quadricep Tendon and Muscle Injury. Uptodate. December 2017
4. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 8th edition. Judith Tintinalli, J. Stapcznski, O. John Ma, Donald Yealy, Garth Meckler, David Cline. 2018. Chapter 274.
5. Watts, Evan. Patellar Tendon Rupture. Ortho bullets. Retrieved April 2 2019. https://www.orthobullets.com/knee-and-sports/3024/patella-tendon-rupture