On a day shift in ambulatory care you receive a 39-year-old woman with foot pain. She was windsurfing when her body was thrown off the board while her foot remained stuck on the board strap. She reported feeling a crack and she is now unable to weight-bear in the emergency department.
Take home points
–These injuries are rare and often misdiagnosed which can lead to significant disability.
-These injuries vary on a continuum ranging from mild sprain to significant fracture-dislocations which can require urgent surgery.
-Look for a characteristic mechanism of injury and specific physical exam findings.
-Consider weight baring views, 30-degree oblique x-ray and CT scan for diagnosis.
The injury was first described by Jacques Lisfranc a field surgeon in the Napoleon’s army when a soldier sustained this particular injury while falling off a horse with his foot caught in the stirrup. The injury is rare (1: 55 000 persons each year) and as many as 20% are missed on initial radiographs.
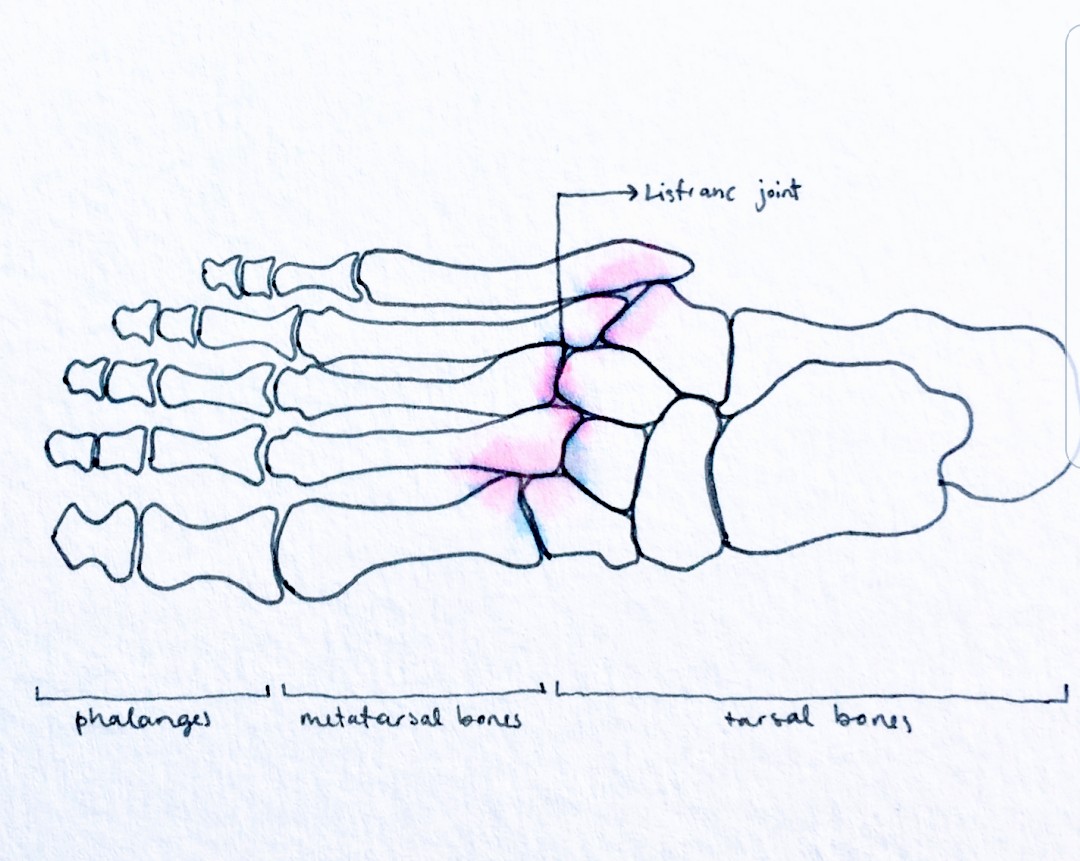
The foot arch is composed of the 3 cuneiform bones, the metatarsal bones and the cuboid. The keystone of this arrangement being the base of the second metatarsal bone. The extent of injuries is highly variable and ranges from ligamentous injury to unstable fracture-dislocations.
Mechanism, symptoms and physical exam
The mechanism of injury involves either an axial loading through a hyper plantar-flexed foot or a crush injury. Often, they are caused by high-energy mechanisms but with the right forces involved, they may also occur with a less stressful mechanism.
The patient often presents with severe pain and is unable to weight-bear, but low velocity injuries may only result in pain with a relatively benign exam. Look for specific clues such as mid foot tenderness, swelling and plantar ecchymosis. Dorsi-flexion, plantar flexion and mobilization of the 1st and 2nd metatarsi in divergent directions often elicit pain. Tarso-metatarsal squeeze (attempting to squeeze the 1st and 5th metatarsi together) may also elicit pain. With significant edema, palpation of the dorsals pedis pulse may be difficult and with severe edema and pain, compartment syndrome should be suspected.
Imaging and diagnosis
Obtain anteroposterior, oblique and lateral views of the foot and consider specific x-ray’s and further imaging if you are suspicious. If the initial x-ray is negative but a high suspicion of Lisfranc injury remains, consider:
If the patient can bear weight:
Bilateral weight-bearing foot x-ray: can show a dynamic displacement in the Lisfranc joint compared to the injured side.
If the patient is unable to bear weight:
Foot CT-SCAN: Can show small avulsion fracture or occult fracture in the Lisfranc joint region.
Note: MRI can help identify a pure ligamentous injury but is rarely done in an ER setting.
Weight-bearing views of both feet can help identify articular incongruence and bone fractures (consider an ankle nerve block for pain control). CT scan can also be helpful for more subtle presentation and pre-operative planning. MRI can help identify purely ligamentous injuries.

Here are x-ray clues of a lisfranc injury
1) Malalignment greater than 1mm:
-On the AP view, the medial border of the 2nd metatarsal should align to the medial border of the middle cuneiform.
-On the oblique view, the medial side of the 4th metatarsal should line up with the medial side of the cuboid.
– On the lateral view, look for any step off of the plantar or dorsal border of the metatarsal bones in relation to the borders of the cuboid and cuneiforms as this is considered abnormal.
2) Look for the Fleck Sign. This is an avulsion fracture over the insertion of the Lisfranc ligament (at the level of the 2nd metatarsal bone and the first cuneiform). This can be seen on the oblique or AP vie.
3) Look for the presence of a proximal metatarsal fracture which should raise your suspicion of an associated Lisfranc injury.
Treatment
In the emergency, once a diagnosis is made, the patient should be made non weight-bearing, put in a posterior slab and have close ortho follow up. If there is any joint displacement, call orthopedics from the emergency as they may require a more urgent surgery. Open reduction with internal fixation (ORIF) or arthrodesis are the two most common operative treatments. Most often soft tissue swelling must resolve prior to operative repair.
Written by: Olivier Saleh, CCFP-EM resident, Mcgill University
Reviewed by: Chanel Fortier-Tougas, Alexis Rousseau-Saine, Daniel Abourbih
References:
“Lisfranc Injury (Tarsometatarsal fracture-dislocation)”. Ortho Bullets. Updated 9/29/2018. https://www.orthobullets.com/foot-and-ankle/7030/lisfranc-injury-tarsometatarsal-fracture-dislocation
Dr. Sayal, Arun. “CASTED Course Manual” 3rd Edition.
Lisfranc Injury, L. Schwartz, N.Tan, J.Costumbrado, JETem (Journal of Education and Teaching, Emergency Medicine), Issue 3:3, last update July 2018
Lisfranc Injury of the Foot: A Commonly Missed Diagnosis, K.E.Burroughs, C.D.Reimer, K.B.Fields, American Family Physician, 1990 Jul 1;58 (1): 118-124
Episode 52: Commonly Missed Uncommon Orthopedic Injuries K.Grewal, I.Cheng, H. Medhian, Emergency Medicine Cases Blog, October 2014