A 13 year old boy present to your ED on a Saturday evening. He was at a birthday party and fell from a table onto an outstretched hand with his left elbow in extension. He is refusing to move his elbow due to pain and you decide to get an x-ray (shown bellow).

In this article, we will describe a 4 steps technique for interpreting a pediatric elbow radiograph.
Take home points
- Using the CRITOE acronym ensure that any free floating bone fragment is an ossification center and not a fracture.
- Look for a posterior fat pad as this is always abnormal and in children it should be treated as a presumed occult supracondylar fracture.
- If the anterior humeral line or the radiocapitellar line is not adequate be suspicious of a fracture
- Document neurovascular status and check for compartment syndrome signs.
Note that it is important to ask for a complete forearm xray in a injured child as a diaphysial and distal radius fracture are commonly associated with elbow fractures.
1. Using CRITOE
In the pediatric elbow x-ray, it can appear as through there are free floating bone fragments. However, what these fragments often represent are up to six ossifications centers that have not yet fused. The ossifications centers consist of cartilage that help to elongate the bone in growing adolescents. They fuse at different ages in boys and girls but can be generalized according the Table 1 below. Using this table, ensure that any free-floating bone fragment is an ossification center and not a fracture. Round edges, localization and sclerotic contours can also help differentiate the ossification centers from actual fractures. Figure 1 shows where the corresponding ossification centers appear on the x-ray. In generally, female ossification centers appear earlier and close earlier then male. If you are unsure about an ossification center, you can x-ray the other joint to compare as they should be similar if the fragments are ossification centers.
Table 1. The acronym CRITOE lists the ossifications in order of appearance.
| Ossification Center | Average Age of Appearance* | Average Age of closure* |
| Capitellum | 1 | 12-14 |
| Radial head | 3 | 14-16 |
| Internal epicondyle | 5 | 16-18 |
| Trochlea | 7 | 12-14 |
| Olecranon | 9 | 15-17 |
| External epicondyle | 11 | 12-14 |
Figure 1: Pediatric Elbow Ossification Centres
Figure 2: Supracondylar Fracture with dorsal fat pad
2. Looking for fat pads
The next step is to check for an anterior or posterior fat pad or « sail sign ». The sail sign is indicative of an intra-articular effusion often related to an occult non displaced fracture of the elbow. In children, we treat them presumptively as a non-displaced supracondylar fracture. An anterior fat pad may be normal if it is small, but a posterior fat pad is always abnormal. Generally, if either is present with a history of trauma, treat for a fracture and have them follow up with orthopedics.
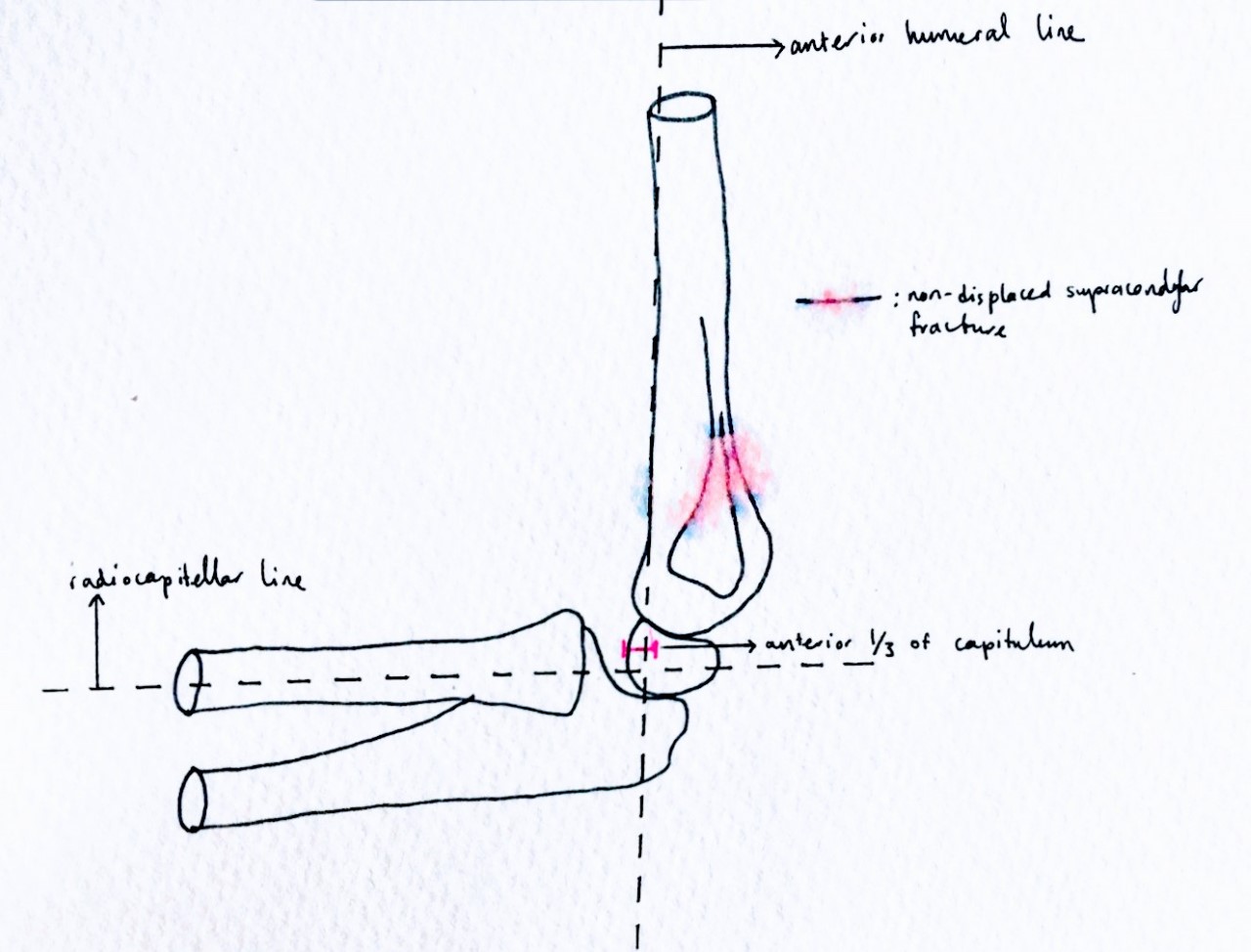
3. Verifying the Radiocapitellar and Anterior Humeral Line
Assess the radiocapitellar line by drawing a line down the center of the radial shaft. This line should bisect the capitellum into two equal parts. If this line is not preserved, this indicates a radiocapitallar subluxation or dislocation, associated with either elbow dislocation or Monteggia fracture (proximal ulna fracture with radial head dislocation).
Assess the anterior humeral line by drawing a line down the anterior aspect of the humerus and this line should transect the middle third of the capitellum (can intersect the anterior third in children < 4 yrs old). If the line lies in the anterior third of the capitellum (in child older than 4 yrs old), or does not intersect with the capitellum, there is likely a displaced supracondylar fracture.
4. The Neurovascular Exam
As with all MSK injuries it is important to examine the patient and document the neurovascular status. Specifically in elbow fractures, check and document radial, median and ulnar nerve function as they can easily be injured. Also, be sure to take and document the radial pulse even if the hand is well perfused. Childrens’ collateral circulation can easily mask a brachial artery injury.
Also, be aware of signs of compartment syndrome of the forearm.
What About This Patient?
If we apply what we have learned to the following example:
- The boy has normal ossifications centers for his age
- He has a posterior fat pad present
- He has a normal radiocapitellar line but an abnormal anterior humeral line
- His neuromuscular exam was normal and he has no evidence of compartment syndrome
This 14 year old boy was therefore treated as a displaced supracondylar fracture
Finally, it is important to remember that the most common elbow fractures in skelettly immature patients as they are different from the adults:
Differential diagnosis of most common elbow fractures in skeletally immature patients (from most to less frequent)
- Supra-condylar fracture
- Radial neck fracture
- Lateral condyle fracture
- Medial epicondyle fracture
- Elbow dislocation
- Monteggia fracture
Written by: Brian Lubelsky, CCFP-EM resident, Mcgill University
Reviewed by: Chanel Fortier-Tougas, Alexis Rousseau-Saine, Daniel Abourbih
References:
- Smithuis R. Elbow fractures in children. Radiology assistant. http://www.radiologyassistant.nl/en/p4214416a75d87/elbow-fractures-in-children.html
- Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 8th edition. Judith Tintinalli, J. Stapczynski, O. John Ma, Donald Yealy, Garth Meckler, David Cline. Nov 10 2018 Chapter : 270.
- Ryan L M. (2017). Elbow anatomy and radiographic diagnosis of elbow fracture in children. UpToDate. Retrieved Nov 12, 2018,
- Woon C, Souder C, Skaggs D. Supracondylar Fracture – Pediatric. Orthobullets. Retrieved Nov 12, 2018 https://www.orthobullets.com/pediatrics/4007/supracondylar-fracture–pediatric